ResistanceMap’s data come from a variety of sources, from small private laboratories in India to large datasets from the European Centre for Disease Prevention and Control, covering 30 countries
Researchers at the Center for Disease Dynamics, Economics & Policy (CDDEP) have released new data documenting alarming rates of bacteria resistant to last-resort antibiotics that can lead to life-threatening infections across the world. Though wealthy countries still use far more antibiotics per capita, high rates in the low and middle-income countries like India, Kenya and Vietnam for which surveillance data is now available sounds a warning to the world.
In India, 57 per cent of the infections caused by Klebsiella pneumoniae, a dangerous superbug found in hospitals, were found to be resistant to one type of last-resort drug in 2014, up from 29 per cent in 2008. In comparison, these drugs, known as carbapenems, are still effective against Klebsiellainfections in 90 per cent of cases in the United States and over 95 per cent of cases in most of Europe.
- See more at: http://indianexpress.com/article/india/data-finally-looks-at-antibiotics-resistance-in-developing-countries-and-figures-for-india-are-scary/#sthash.ZsE1ZZyA.dpuf
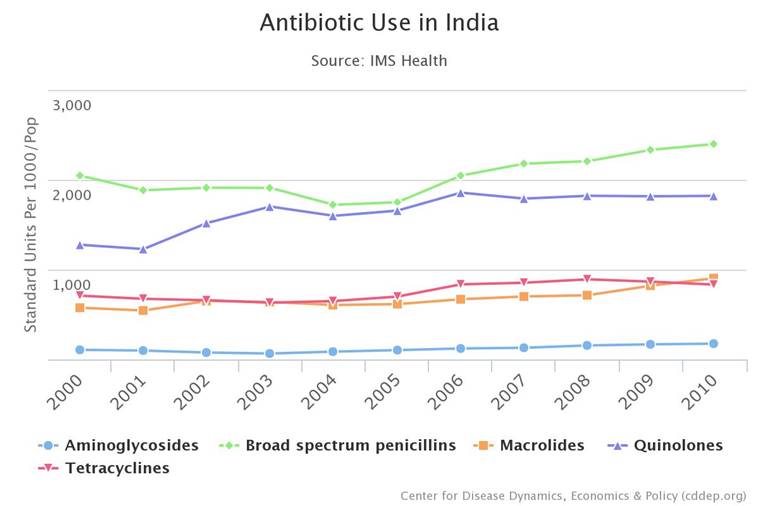
The findings were released via CDDEP’s ResistanceMap, an interactive online tool that allows users to track the latest global trends in drug resistance in 39 countries, and antibiotic use in 69 countries. It includes infections caused by 12 common and potentially deadly bacteria, including Escherichia coli (E. coli), Salmonella, and methicillin-resistant Staphylococcus aureus (MRSA). This is the first time data from a significant number of developing countries have been brought together publicly. CDDEP also issued the first report to look comprehensively at the current state of global antibiotic use and drug resistance in humans, livestock and the environment. The report, The State of the World’s Antibiotics 2015, lays out six strategies that belong in every national plan to halt the spread of resistance. Authors say antibiotic stewardship is the key component of that action, and they challenge the frequently-cited notion that the problem with antibiotic resistance is a lack of new drugs in the antibiotic pipeline. Between 2000 and 2010, total global antibiotic consumption grew by more than 30 per cent, from approximately 50 billion to 70 billion standard units, based on data from 71 countries, including most high-population countries. Per capita consumption is generally higher in high-income countries, but the greatest increase in antibiotic use between 2000 and 2010 was in LMICs, where use continues to rise. Carbapenems are considered last-resort antibiotics, used for infections that are resistant to first, second and even third line antibiotics. New findings indicate that Klebsiella pneumonia resistance to last resort antibiotic class carbanpenems was 57 per cent in India in 2014, up from 29 per cent. In Europe this number is less than 5 per cent. In India, this is a very dangerous trend, because Klebsiella resistance to a variety of drugs is high. The super bug found in hospitals is around 80 percent resistance to the drug class third generation cephalosporins, 73 per cent resistant to fluoroquinolones, and 63 percent to aminoglycosides. “For four of five drug classes tested, Klebsiella was more than 60 percent resistant in India,” Dr Ramanan Laxminarayan, CDDEP Director and report co-author, when contacted in New Delhi told The Indian Express. This new data provides global trends in drug resistance in 39 countries and antibiotic use in 69 countries and documented alarming rates of bacteria resistant to last-resort antibiotics that can lead to life-threatening infections across the world. It includes infections caused by 12 common and potentially deadly bacteria, including Escherichia coli (E. coli), Salmonella, and methicillin-resistant Staphylococcus aureus (MRSA). This is the first time data from a significant number of developing countries have been brought together publicly. E. coli resistance is high and rising for many drug types and in many world regions, according to ResistanceMap. But compared to all other countries, India has the highest rates of resistance to nearly every drug used to treat it; strains of E. coli are more than 80 per cent resistant to three different classes of drugs, meaning treatment options are becoming increasingly limited. “Carbapenem antibiotics are for use in the most dire circumstances—when someone’s life is in danger and no other drug will cure the infection,” said Sumanth Gandra, a CDDEP resident scholar in New Delhi. ResistanceMap also tracks rates of antibiotic use, and findings indicate that both human and animal antibiotic use is rising dramatically in middle-income countries—particularly China, India, Brazil and South Africa. In many countries, antibiotics are easily purchased in pharmacies and shops without prescription. “A rampant rise in antibiotic use poses a major threat to public health, especially when there’s no oversight on appropriate prescribing,” said Laxminarayan. “Antibiotic use drives antibiotic resistance.” ResistanceMap’s data come from a variety of sources, from small private laboratories in India to large datasets from the European Centre for Disease Prevention and Control, covering 30 countries. ResistanceMap, supported by a grant from the Bill & Melinda Gates Foundation, says limiting overuse and misuse of antibiotics are the only sustainable solutions. “India is represented by data from SRL, a large private laboratory network from 2008 to 2014. This network includes 5,700 collection centers in 26 of India’s 29 states and two of seven Union Territories. The collection centers include private hospitals (tertiary care, secondary care) and diagnostic laboratories; samples are also collected in patients’ home. Efforts are underway to expand the ResistanceMap network to include other large private laboratories and both private and public hospitals in India, Dr Ramanan said. In order to to strengthen the surveillance of antimicrobial surveillance in the country, the Indian Council for Medical Research, has been tracking resistance pattern of six pathogens causing diarrhoea, typhoid, fungal infections and infections that patients acquire in hospitals and ICUs. It has set up six nodal centres in four hospitals at PGI, Chandigarh, Christian Medical College, Vellore and one each at AIIMS, New Delhi and JIPMER in Pondicherry. - See more at: http://indianexpress.com/article/india/data-finally-looks-at-antibiotics-resistance-in-developing-countries-and-figures-for-india-are-scary/#sthash.ZsE1ZZyA.dpuf

